Introduction: Neutrophils play a crucial role in sepsis by releasing neutrophil extracellular traps (NETs), webs of DNA complexed with histones and antimicrobial proteins that capture pathogens and prevent bacterial dissemination. However, whether or not NETs are capable of killing bacteria remains controversial. Our group has preciously shown that the positively charged, platelet-specific chemokine, platelet factor 4 (PF4, CXCL4), binds to NETs, enhancing NET resistance to nuclease digestion and markedly increasing their ability to capture bacteria. In this study, we investigate the heterogeneity of in vitro NET bactericidal ability between donors, and examined whether PF4-NET binding modulates NET antimicrobial functions.
Methods: Neutrophils (2-3x10 7/mL) were purified from healthy donors (n=4) and treated with phorbol-2-myristate-13-acetate (100nM) for 4 hours at 37°C to produce neutrophil-adherent NETs, which were cleaved from cell bodies by treatment with a low dose of DNase I (4 U/mL), yielding NETs >50 kilobase pairs (bp) long. Additional treatment of NETs with DNase I (100U/ml) for 1h at 37°C generated smaller NET fragments (<250bp). K12 Escherichia (E) coliwere grown in lysogeny broth until bacteria culture has reached the log-growth phase (OD 600=0.4). Intact or degraded NETs were pre-treated with PF4 (0-100µg/ml) for 20min at 37°C, and then exposed to E coli (5x10 8/mL) for 20min at 37°C. Samples were plated on agar plates, and colony forming units (CFUs) were counted at 24 hours. Baseline levels of PF4 and antimicrobial peptides myeloperoxidase (MPO) and matrix metallopeptidase 9 (MMP9) were measured in DNase I-digested NETs (n=4) using commercial ELISA kits.
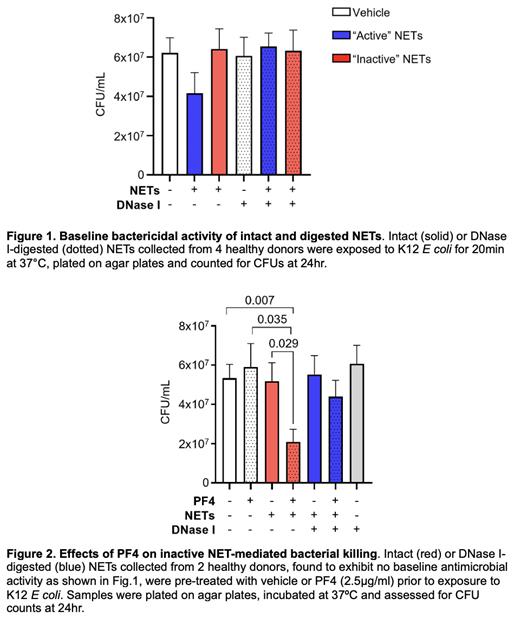
Results: Baseline differences in the bactericidal potential of intact NETs were observed between different donors. Half of the examined intact NET samples (n=2; labeled as “active” NETs) exhibit baseline bactericidal activity, with killing of ~20% of bacteria, whereas the other half of NET samples (n=2; labeled as “inactive” NETs) did not prevent bacterial proliferation ( Fig. 1). In inactive NETs, the addition of PF4 at 2.5µg/ml, a concentration readily achieved in the setting of platelet activation, increased NET bactericidal capacity by 2.5-fold ( Fig. 2). NET digestion with the nuclease DNase I, abrogated the inherent bactericidal effects of active NETs ( Fig. 1). PF4 treatment of digested NETs did not restore bacterial killing ( Fig. 2). To investigate the hypothesis that differences in PF4 contamination or variation in concentrations of neutrophil granular proteins could be influencing NET bactericidal capacity, we measured NET levels of PF4 and the antimicrobial proteins MPO and MMP9. Although there was variation in NET concentrations of PF4, MPO, and MMP9 between donors, these differences were not associated with changes in bacterial killing.
Conclusions: We observed heterogeneity in bactericidal capacity between NETs isolated from different donors, with active NETs killing bacteria at baseline, and inactive NETs killing bacteria following incubation with PF4. We demonstrate for the first time that PF4 interacts with NETs to enhance their ability to capture and kill E coli. Studies are underway to identify which components influence the antimicrobial properties of NETs, and will include quantification of histones, defensins, and neutrophil elastase. These results will help to define the mechanism by which PF4 augments NET antimicrobial function.
Disclosures
No relevant conflicts of interest to declare.